Stroke: How to protect & preserve your brain
rocketclips - stock.adobe.com.
Each year, 795,000 people in the US have a stroke, and 165,000 die due to a stroke. Half of US adults—and 75 percent of those aged 65 or older—have high blood pressure, the strongest risk factor for a stroke. Here’s what to know.
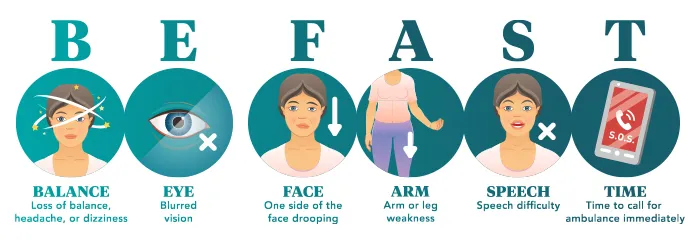
1. Signs of a stroke? Call 911
Feeling weak or numb in one arm or leg? Having trouble speaking or seeing? It’s tempting to ask someone to drive you to the hospital or to wait to see if your symptoms fade.
Don’t. Call 911 instead. Why?
“The benefits of emergency treatment for an acute stroke decrease with the amount of time the brain is starved of blood and oxygen,” explains Larry Goldstein, chair of the department of neurology at the University of Kentucky.
“Time saved is brain saved.”
And treatment can start sooner if the hospital is ready for you.
“Calling 911 brings immediate first responders who can notify the hospital to prepare for you and bypass waiting rooms to get you to the care you need without delays,” says Goldstein.
Or the ambulance might bring you to a hospital that’s farther away but better equipped to treat strokes.
“Calling 911 ensures rapid transport to the most appropriate hospital,” says Goldstein.
Another reason not to ignore symptoms that disappear within an hour or so: You may have had a transient ischemic attack—that is, a temporary blockage of blood flow to the brain.
“The typical signs or symptoms of a transient ischemic attack—or a TIA, also called a mini-stroke or maybe a warning—are the same as that of a real stroke,” noted Hardik Amin in 2023, when he chaired an American Heart Association panel that issued advice on diagnosing TIAs. (Amin is now co-director of the Comprehensive Stroke Center at Hartford Hospital in Connecticut.)
And nearly one in five people who have a suspected TIA will have a full-blown stroke within three months. Nearly half of those strokes will happen within two days.
What’s more, with the appropriate brain scans, two in five people with a suspected TIA will learn that they actually had a stroke instead of a TIA.
One more reason to call 911: Doctors can now undo some of the damage caused by a stroke...but only if you get to the hospital in time.
2. We’ve had a revolution in stroke care
“The first revolution in stroke care came with studies showing that treatment with clot-busting drugs greatly improved outcomes in selected patients having a stroke,” says Goldstein, who is also co-director of the Kentucky Neuroscience Institute.
Blood clots in the brain cause 87 percent of strokes in the U.S. (Those are called “ischemic.” The rest are due to a hemorrhage.) And since 1996, doctors have used tissue plasminogen activator (tPA) to break up the clots.
The catch: tPA should be administered within 4½—and ideally, 3—hours after the first signs of a stroke. “Even within that time frame, the sooner, the better,” says Goldstein.
And doctors can’t start until they get a CT scan to make sure that the stroke wasn’t caused by a hemorrhage.
But tPA has its limits. It works best for blood clots in the brain’s smaller blood vessels.
“Its benefit was less in those who had a big clot closing a larger brain blood vessel,” acknowledges Goldstein. And that matters.
“Almost 40 percent of acute ischemic strokes are due to a large vessel occlusion,” explained Bart Besinger, an associate professor of clinical emergency medicine at Indiana University, in a training video for emergency-department doctors.
What’s more, added Besinger, “the bigger the vessel the stroke is in, the worse that patient is going to do. These are the bad strokes.”
That led to the next revolution in the war on strokes. Rather than break up the big clots in big blood vessels, doctors now simply take them out.
“With mechanical thrombectomy, a tube is put into the blood vessel to remove the clot,” explains Goldstein. The tube uses either suction or a wire mesh to pull the clot out.
“That was proven to greatly improve outcomes,” adds Goldstein.
But doctors need to do a certain type of brain scan to see if you need a mechanical thrombectomy, and some hospitals aren’t equipped to do them.
“Again, time is critical,” says Goldstein.
A thrombectomy is ideally done within six hours after stroke symptoms start. However, in two later trials, the procedure also helped people who had “wake up strokes”—that is, they were last symptom-free up to 16 or 24 hours earlier, and their symptoms may have started while they were asleep.
That doesn’t change the takeaway: Every minute counts.
“A meta-analysis in JAMA Neurology...looked at patients with an acute ischemic stroke due to a large vessel occlusion who had mechanical thrombectomy performed within four hours,” recalled Besinger.
“For every 10-minute delay in time to mechanical thrombectomy, that patient lost, on average, 1.8 months of healthy [life].”
How a stroke can start
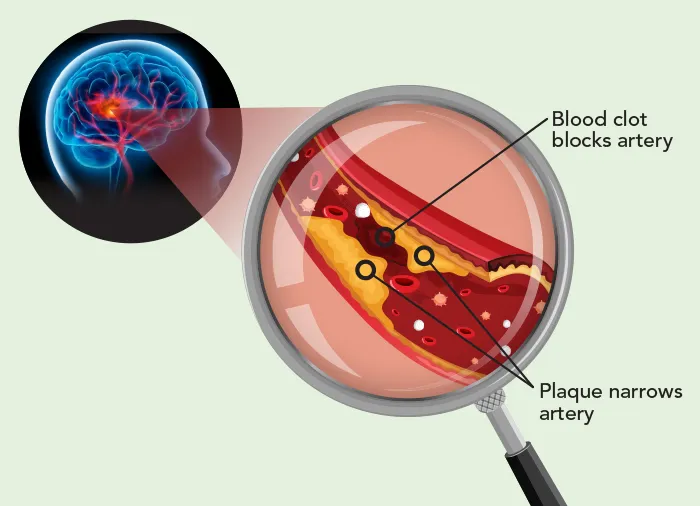
Ischemic strokes often occur when a large blood clot gets stuck in an artery that’s partially clogged by plaque. Doctors may insert a tiny tube into an artery in the leg and use suction or a wire mesh to remove the clot.
3. Women may have extra risks
Men have a higher risk of stroke in young and middle age, but more women die of a stroke. That’s partly because women typically live longer. But it’s also because some conditions put them at greater risk.
A few examples:
Atrial fibrillation
“Women with atrial fibrillation have a higher risk of a stroke caused by a thromboembolism than men,” says Cheryl Bushnell, professor of neurology at Wake Forest University School of Medicine.
How can atrial fibrillation—an irregular heart rhythm in the upper chambers (atria) of the heart—cause a blood clot that may travel to the brain? If blood isn’t efficiently pumped out of the atria, what’s left behind can pool and form blood clots, which can travel to the brain.
“Treating people who have AFib with anticoagulant medications leads to a huge reduction in stroke risk,” notes Bushnell, who chaired the panel that wrote the American Heart Association’s 2024 Guideline for the Primary Prevention of Stroke.
Early-onset menopause
Women who go through menopause before age 45 have a greater risk of stroke.
“Estrogen helps keep blood vessels functioning normally, so if a woman is deprived of estrogen earlier than normal, it can have detrimental effects on the blood vessels,” says Bushnell.
But taking estrogen after menopause may increase stroke risk. Why?
“If a woman smokes or has had high blood pressure, high cholesterol, or diabetes, their blood vessels are stiffer, they’ve got plaque in them,” explains Bushnell. “When you add estrogen to that, you increase the risk of more plaque and more clots.”
Endometriosis
“When uterine tissue is found outside of the uterus, it causes inflammation, so you have a lot of inflammatory factors floating around in the abdomen and ultimately in the bloodstream,” says Bushnell. “That inflammation can increase the risk of heart attack and stroke.”
Migraine headaches
“Migraines increase the risk of stroke, especially migraines with aura,” says Bushnell.
“That’s the bright or flashing lights that some people see before the headache. And migraines are more common in women.”
4. Blood pressure matters most
When it comes to stroke, one risk factor stands out: high blood pressure.
“To prevent plaque development and lower the risk of a stroke or heart attack, the body likes systolic blood pressure as low as it can get,” says Paul Whelton, professor of epidemiology at Tulane University and former dean of its School of Medicine and its School of Public Health and Tropical Medicine.
“The data are very compelling.”
Whelton ought to know. He co-led the SPRINT trial, which randomly assigned people with hypertension to aim for a systolic blood pressure below either 140 or 120.
The trial was stopped early—after only three years—when it became clear that the 120 group had a 34 percent lower risk of a heart attack, stroke, or other cardiovascular event than the 140 group.
Based on SPRINT’s results, Whelton chaired the expert panel that redefined “high” and “elevated” blood pressure. He recently analyzed seven trials looking at blood pressure’s impact on stroke or heart attack risk.
“Getting to less than 140 is critically important if your blood pressure is at a higher level,” he says. “You get additional benefit as you get below 130, and even more if you go down to 120 or lower.”
And many of us are above 120.
“At every decade of life, the average blood pressure marches upward,” says Stephen Juraschek, associate professor of medicine at Beth Israel Deaconess Medical Center in Boston. “Ninety percent of adults develop hypertension over their lifetime.”
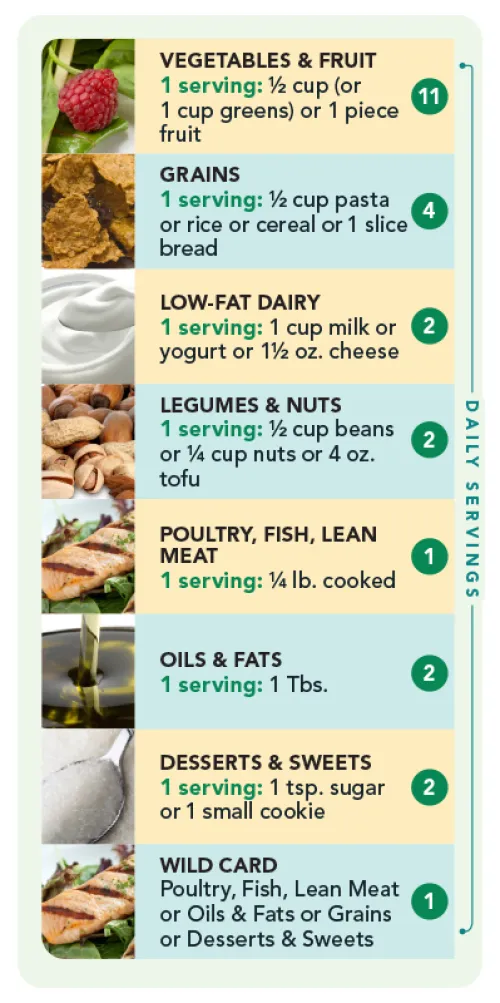
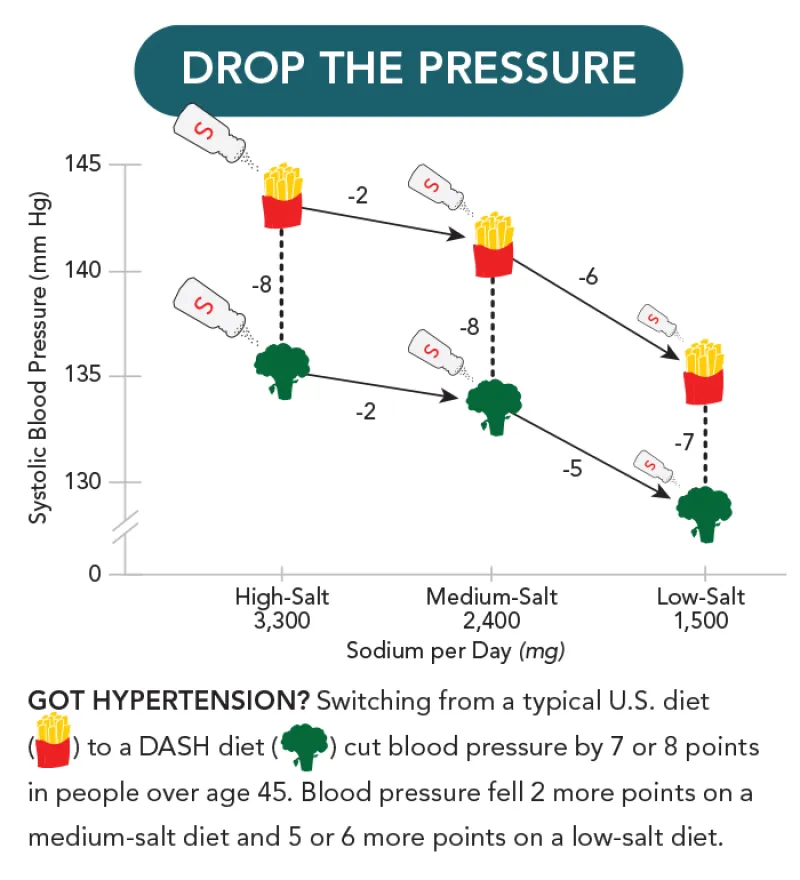
The good news: Diet can help lower blood pressure, whether or not you also need medications. Two key strategies: cutting sodium and eating a DASH (Dietary Approaches to Stop Hypertension) diet.
“If you started with a systolic blood pressure of 150, it could drop as much as 20 points,” says Juraschek. “That’s on par or greater than some medications.”
Cutting sodium lowered blood pressure more in older people than in younger people. Why?
“Older people may have reduced kidney function, making it harder to excrete sodium,” suggests Juraschek.
What might explain how the DASH diet trims blood pressure? Its fruits, vegetables, and low-fat milk and yogurt are rich in potassium.
“Potassium works in the kidneys to help the body dump sodium,” explains Juraschek.
And the DASH diet replaced most red meat with fish, poultry, beans, and nuts. It also limited sweets.
“So DASH targeted multiple different pathways to lower blood pressure,” Juraschek points out.
In OmniHeart, a later trial, researchers replaced some of DASH’s carbs with healthy protein or with unsaturated fats, making it more like a Mediterranean diet. That nudged blood pressure down another three points or so. And it’s not just lower blood pressure.
“We’ve shown direct effects of DASH on a biomarker of subclinical cardiac injury and a biomarker of inflammation,” says Juraschek. He’s talking about high-sensitivity cardiac troponin, a sign of heart muscle damage, and high-sensitivity C-reactive protein.
“These markers were reduced even in the short 12-week duration of the DASH-Sodium trial,” says Juraschek.
Do the DASH
Load up on fruits and vegetables and cut back on salt, bad fats, and added sugars. Here’s a 2,100-calorie version of a DASH-OmniHeart diet mix. (Note: servings are small.) Add the “Wild Card” you prefer.
5. Strokes can cause cognitive decline
It’s no surprise that a stroke can take a toll on your mind.
“A severe stroke can increase the risk of dementia 50-fold,” says Deborah Levine, professor of medicine and neurology at the University of Michigan Medical School.
In one study, one out of three stroke patients had developed dementia after five years.
The impact is worse on older people. Why? “Older adults have less cognitive reserve to withstand a brain injury due to existing neurodegeneration,” explains Levine.
And 10 to 20 percent of adults may have had so-called silent strokes.
“If you do CT scans or MRIs, you find a bunch of people who have had strokes and were never aware of it,” says Tulane’s Paul Whelton.
What’s more, high blood pressure is a threat to your mind even if you never have a stroke. That link is clear in studies that track thousands of people for years.
“In observational studies, hypertension, particularly in midlife, is a major risk factor for dementia and cognitive impairment,” says Levine.
The SPRINT-MIND trial yielded stronger evidence in older adults.
“In that landmark trial in older adults at high risk for cardiovascular disease, lowering blood pressure to 120 reduced the risk of mild cognitive impairment,” notes Levine.
(SPRINT-MIND saw no difference in dementia, its primary outcome, possibly because the trial was cut short after only three years.)
How might hypertension cause dementia?
“Is it purely injury to blood vessels or does it increase or trigger the amyloid or tau deposition seen in Alzheimer’s disease, or is it other mechanisms, including inflammation?” asks Levine. “It’s hard to say.”
Her takeaway: If you’re 40 or older, don’t wait a year between doctor’s visits to check your blood pressure.
“Get an accurate home blood pressure monitor and take your pressure twice daily for at least one week a month, with morning and evening readings,” advises Levine.
“We have no current treatments that can prevent or stop dementia. Diagnosing and treating high blood pressure early and effectively is a strong strategy to reduce dementia and cognitive impairment independent of stroke.”
How to cut your risk of a stroke

Treat high blood pressure. High blood pressure helps clog arteries and damages blood vessel walls.
Lower LDL cholesterol. High LDL (“bad”) cholesterol can narrow or clog blood vessels in the brain.
Manage diabetes. High blood sugar can damage blood vessels in the brain.
Don’t smoke. Smoking cigarettes helps clog arteries, promote blood clots, and damage cells that line blood vessels.

Lose excess weight. Expect about a 1-point drop in pressure for every 2 pounds you lose.
Keep moving. Aim for both exercise (like brisk walking for 150 minutes a week) and not sitting for more than 11 hours a day.
Eat a DASH-like diet. Cover half your plate with fruits or vegetables. Fill the rest with low-fat dairy and beans, nuts, fish, poultry, and healthy fats.
Limit sodium. Deli meats, soups, sandwiches, pizza, frozen dinners, and restaurant foods are some of the worst offenders.
Limit alcohol. The more you drink, the higher your risk. Aim for no more than 1 drink a day (for women) or 2 drinks a day (for men).

Don’t rely on supplements. In clinical trials, vitamin D, fish oil (EPA & DHA), antioxidant vitamins (E, C, and beta-carotene), and B vitamins failed to lower stroke risk.
Get a home blood pressure monitor. Go to validatebp.org to find a reliable blood pressure device.
Support CSPI today
As a nonprofit organization that takes no donations from industry or government, CSPI relies on the support of donors to continue our work in securing a safe, nutritious, and transparent food system. Every donation—no matter how small—helps CSPI continue improving food access, removing harmful additives, strengthening food safety, conducting and reviewing research, and reforming food labeling.
Please support CSPI today, and consider contributing monthly. Thank you.
More on stroke
A snapshot of the latest research on diet, exercise, and more
Healthy Eating

CSPI urges Congress to remove industry-serving riders blocking progress on sodium reduction from FY24 Appropriations Bill
Government Accountability

Could Ozempic curb heart attacks & strokes?
Weight and Health

The 10 leading causes of death in the United States
Preventing Disease

A new reason for older adults to get the shingles vaccine
Preventing Disease


